HealthANSWERS partnership
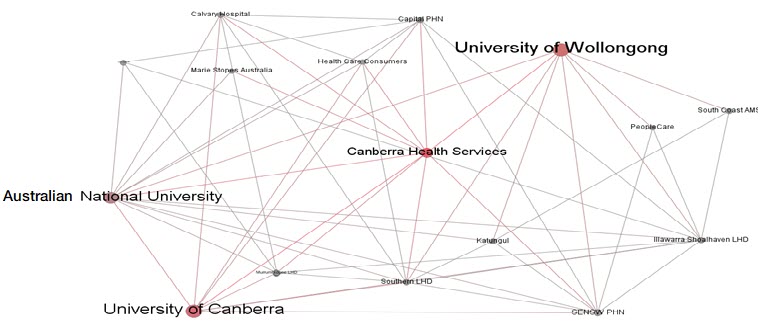
The HealthANSWERS (ACT, NSW Education, Research and Service) Partnership is an established network of healthcare services, support agencies and major universities in the ACT and southern New South Wales that provides unparalleled opportunities to develop, pilot and implement health promotion and healthcare improvements.
Our vision
Universal access to optimal healthcare and health promotion – high-quality, high-value, timely, and close to home - through integration of primary and specialist services, supported by healthy community initiatives, and demonstrated in a powerful population-level ‘living laboratory’ that enables rapid learning healthcare systems, and design, piloting and refinement of health system innovations.
Who we are
The HealthANSWERS (ACT, NSW Education, Research and Service) Partnership is an established network of healthcare services, support agencies and major universities in the ACT and southern New South Wales that provides unparalleled opportunities to develop, pilot and implement health promotion and healthcare improvements. The Partnership builds on a decade of service-oriented research and education between the participants to address pressing challenges in regional health care: ensuring quality of care across diverse and isolated settings; building and maintaining a sustainable workforce; navigating complex transitions across borders and between primary and tertiary care; and providing sufficient infrastructure and support to generate evidence for practice improvement.
Our Partnership has developed as a population-based system for innovations to improve regional health and healthcare delivery. This system can be conceptualised as having ‘layered’ attributes and capabilities, which in turn enable focused research and education initiatives on national imperatives such as mental health, cardiovascular disease prevention, cancer, multimorbid illness, digital health, and primary care policy (the ‘pillars’ in Figure 1).

The region for the Health Partnership incorporates the ACT, and regional NSW in southern NSW. This includes three NSW Local Health Districts (Shoalhaven/Illawarra, Murrumbidgee and Southern NSW), and three PHNs (Murrumbidgee, COORDINARE, and ACT): approximately 1.2 million people, many of whom travel regularly and across borders for health care.
Members of the partnership
Our health sector partners are
- Canberra Health Services
- ACT Health Directorate,
- ACT Ambulance Service
- Southern NSW Local Health District,
- NSW Ambulance Service,
- Calvary Hospital Bruce ACT,
- ACT Primary Health Network,
- Health Care Consumers Association,
- Illawarra Shoalhaven Local Health District,
- Katungul Aboriginal Corporation Regional Health and Community Services,
- Murrumbidgee Local Health District,
- Murrumbidgee Primary Health Network,
- SENSW Primary Health Network,
- South Coast Medical Service Aboriginal Corporation
Our industry partners are Canberra Innovation Network, Social Research Centre, Marie Stopes Australia, Medcast Pty Ltd, NPS Medicinewise, Peoplecare Health Ltd, Telstra Health and Thrivor Pty Ltd.
Academic partners already interact extensively with these service networks, and include the Australian National University, CSIRO Health and Biosecurity, University of Canberra and University of Wollongong
The interlinkages over the last ten years are illustrated below.
Our history and our work
Our work draws on 10 years of service-based research in the region by current and predecessor organisations. All the universities have histories of collaboration with each other and with the services in the region. Approximately one third of all clinicians in the region are associated with at least one of the three universities, as field supervisors or research collaborators.
Vertical integration of research, education and patient care
The three universities between them train students in twelve different health care disciplines, who upon graduation are often employed within the HealthANSWERS footprint. The universities have unusually broad experience with vertical integration of their education into vocational, or post-professional, education for clinicians in the region.
Horizontal integration of research, education and patient care
The footprint of the HealthANSWERS Partnership covers 18 rural sites of education for pre-vocational medical, nursing and allied health students, most of which have their own on-site teaching facilities and administrative support, and can be used for post-vocational and continuing education. ANU and UC have collaborated on enhancing teaching support in regional hospitals in South East NSW, and the educational hubs in Bega, Young, Cowra, Goulburn and Moruya used for university education of medical students can be and are sites of interprofessional activity. These interdigitate with UOW clinical placements in the Shoalhaven, Bateman’s Bay, Bega and Griffith, enabling streamlining of education, and enhancing interprofessional education. In addition, UC and ANU have invested in a large joint infrastructure project, building training facilities on hospital land in Bega, Cooma and Moruya which will facilitate inter-professional learning not only of students but also of staff, and enable the in situ building of research capacity of staff in the region. The SENSW Regional Training Hub, administered by the ANU Rural Clinical School, provides additional support to improve sustainability of the rural workforce through expansion of accredited positions for subdisciplinary training and support for clinical supervisors.
Our positioning of consumers as foundational (“Nothing about us without us”) is demonstrated through their presence on the HealthANSWERS Council and on its working committees.
What our partnership does
The HealthANSWERS Partnership focuses particularly on health systems research, drawing together the strong translational knowledge platforms in the university partners in the areas that link the operation of primary care with specialist knowledge and expertise in prevention and early intervention of common chronic diseases. We will map health eco-systems and population health planning, policy translation, preventive health (especially for common cancers and obesity complications), precision medicine, health economics, data analytics for health decision making, health communications research, and AI systems.
The partnership is underpinned by a philosophy that rural and regional Australia, under principles of equity and logistics of health economics, must be included in new developments in medicine and medical practice. Effective preventive health care and best standards of early intervention can, with imaginative planning and strategic/efficient links be made to operate in cities, smaller towns, city-proximate and remote urban communities. Key systems areas to improve the translational service platforms will be strengthening primary care, integrating care better from primary to tertiary care, cross-disciplinary models of care, enhanced remote service delivery for specialist services, and preventive care in and for communities.
Health sector partners have identified the following areas for focused initiatives of importance to them:
- Mental health care and community support initiatives
- Multi-morbid illness, including psychological co-morbidity
- Cancer prevention and care: particularly colorectal and liver cancer
- End of life care
The health partnership underpinning the Centre already delivers translational research in many of these clinical areas.
Exisiting research
Mental health care
Our mental health service and systems leadership in the region exemplify our multi-level, cross-disciplinary, evidence-led clinical care and policy-making. There is a recognised need for enhanced community-based mental health services, community care and preventive programs aimed at mental health literacy, suicide prevention and community connectedness. Examples include:
- The new MIND the GaP facility, a collaborative venture between UOW, Lifeline and Shoalhaven City Council, with extensive community engagement, located on the Shoalhaven campus of UOW: this facility provides mental health care services via Lifeline, and research aimed at improving mental health services and outcomes in rural NSW, with a focus on Indigenous mental health. (https://www.uow.edu.au/mind-the-gap/index.html).
- Investigation into optimal care pathways for people with Borderline Personality Disorder (Ms Judy Pickard, ISLHD)
- Suicide prevention program Way Back Support Service (Beyond Blue, ACT Health): provides trauma-informed non-clinical care to individuals for 12 weeks after a suicide attempt. The ACT hosted one of the trials and the program is now being rolled out nationally. Health Care Consumers’ Association worked with consumers to improve the service and inform the national model. Associate Professor Phil Batterham, ANU Centre for Mental Health Research developed outcome measures for the national evaluation.
- Research School of Psychology, ANU: runs supervised eClinics as part of training for clinical psychologists, extending into SENSW, as a direct response to the need for remote access to clinical psychology in this region.
The service and systems research described above is at present integrated into the work of the commissioning health services. Future plans of the Partnership are to expand and translate novel programs and collaborative community wellness initiatives to other regions, particularly from the UOW MIND the GaP initiative; and to formulate better policy for farmers facing challenges to sustainable living and mental health, led by Dr Batterham ANU. In 2019 the ACT kindergarten screening program, in existence for more than 15 years, will begin collecting data on children’s emotional health through a Strengths and Weaknesses questionnaire. For the first time this will enable scoping of children’s wellbeing and will complement the cutting-edge work on early childhood health led by Professor Anthony Okely at UOW’s Early Start facility.
Cancer care
Cancer care in SE NSW and in part of the Murrumbidgee region is delivered through outreach clinics and local collaborative services by Canberra Health Services. Thirty percent of people accessing cancer services at the Canberra Region Cancer Centre (CRCC), and half those requiring acute and complex surgery, are from NSW. Under the ACT and Southern NSW Local Health District Cancer Services Plan (2015-2020), joint appointments of clinicians from Southern NSW LHD and Canberra Health Services are made to support best practice approaches and enable multidisciplinary Canberra-based teams to provide advice across the region. They are supported by the ACT & SE NSW Breast Cancer Treatment Group, which has conducted quality audits on regional breast cancer care for over 20 years. Similar initiatives provide high quality cancer care in the ISLHD footprint with integrated cancer care services in Wollongong and Nowra. Examples of how locally generated clinical problems drive research to benefit regional patients are the phase 1 trial of infusion-friendly 5-flurouracil and leucovorin for the treatment of colorectal cancer, a collaboration between Professor Philip Clingan (ISLHD) and Professor Marie Ranson (UOW/IHMRI), and novel drug delivery systems to treat pancreatic cancer (Professor Morteza Aghmesheh, ISLHD).
The Canberra Region Cancer Centre collaborates with the Kinghorn Cancer Centre (Garvan Institute of Medical Research) on the MosT (Molecular Screening and Therapeutics) Clinical Trial and the Australian Genomic Cancer Medicine Program, supported by $50 million in Australian Government funding over five years. These research projects are built around cutting-edge molecular and genetic analysis of rare currently incurable tumours (collectively, a large cancer burden) to identify therapeutic targets. Both of these initiatives enable patients to have samples and information submitted to the Kinghorn Centre for analysis, and have potential therapies identified and delivered locally.
Cancer patients in our region participate in early phase clinical trials of new interventions to alleviate symptoms, or as a ‘last hope’ for disease that has not responded to standard care or for which no curative treatment exits. Currently patients in our region must travel to Sydney or Melbourne to participate in Australian phase I trials. Future plans for evidence-based cancer care involve a collaboration with the Peter MacCallum Cancer Centre, Garvan Institute and the Australian Genomic Cancer Medicine Centre. This partnership (led by Professor Ross Hannan) will work with Canberra Clinical Genomics to use genomics to improve the early detection, prevention and management of cancer, sealing the translation cycle between clinical trial and health care improvement within the HealthANSWERS Partnership footprint. A specific opportunity for brain cancer translational research is offered by our collaboration with the NIH “Brain Cancer Moonshot Initiative” funded by the US Federal Government, which represents the world’s largest network of collaborative brain cancer clinicians. In 2018, we developed a pipeline for Australian patients with brain cancer to enter the US trials, led by Dr Leonie Quinn, ANU JCMSR. This includes funding from the NIH Moonshot project to cover patient and carer costs for travel in the US, accommodation and treatment for the duration of the trial. Several patients have already been referred for assessment by ACT neuro-oncologists.
Obesity and co-morbidity
Obesity is identified by the health sector partners as one of the most pressing health problems in the region, associated with multiple co-morbidities. The Australian Geospatial Health Research Hub (AGeo-H), a partnership between the University of Canberra and GIS industry leader Esri to support population research applying spatial epidemiology to understand and prevent chronic disease. AGeo-H enables the elucidation of built, social, natural and physical environmental factors to be targeted by policy and practice-level innovations to reduce risk factors and treatment costs arising from obesity, metabolic syndrome, diabetes, cardiovascular diseases and cancers. The UC Centre for Research and Action in Public Health also administers the annual rural health survey to all rural NSW, generating data used by Primary Health Networks in their reporting and prioritising of different health issue
End of life care
Although most people in the HealthANSWERS region wish to die at home, over half die in rural hospitals or palliative care facilities. The Advance Project, led by Professor Elizabeth Halcomb (UOW) and Dr Joel Rhee (UOW) produced a practical, evidence-based toolkit of screening and assessment tools and a training package, designed to support Australian general practices to use teams to initiate advance care planning and palliative care in everyday clinical practice. The SE NSW Primary Health Network is working with ANU Rural Clinical School and Department of Health Services Research to trial safe anticipatory prescribing by GPs in aged care settings for palliative care in rural NSW. Palliative care specialists Dr Michael Chapman and Ms Nikki Johnson (Canberra Health Services, Calvary Hospital) have developed a checklist that improves the quality of care, provides staff with focused case-based education, maximises planning and reduces symptom burden for aged care residents at end of life. The introduction of Palliative Care Rounds led by palliative nurse practitioners has been demonstrated to substantially reduce the length of hospital stays and lower the incidence of death in the acute care setting.
Future plans for end-of-life care include consolidation of rural and urban initiatives, drawing on a collaboration led by Professor Imogen Mitchell, ANU, with the Australian Commission on Safety and Quality in Health Care, describing the dying process in eight hospitals (1600 patients and perceptions of 4000 healthcare professionals). This work will be supported by the expanded Palliative Care Outcome Collaboration datasets at UOW capturing palliative care outcomes in primary care, aged care and intensive care (led by Professor Kathy Eagar, UOW), and translated into health service outcomes through The Advance Project (UOW) and the ACT End of Life and Palliative Care Collaborative.
For more information about HealthANSWERS, visit the dedicated website:
Engage with us
Contact a Course Advisor Make an enquiry
Plan a visit Give to ANU